You’ll work in small groups facilitated by practicing doctors following a 'problem based learning' curriculum. This often starts with the problems patients bring to you, and means you will learn about health from both the doctors’ and patients’ perspective.
We are still open to applications from international students for September 2026 entry.
Overview
Our MBChB (Bachelor of Medicine and Bachelor of Surgery) programme will prepare you to become a medical doctor. With further training you can practice in any specialist area, from General Practice and Public Health, to Psychiatry, Anaesthesia and Surgery.
At Worcester, you’ll spend much of your time learning medicine in the community alongside patients, as well as studying on campus. You’ll work closely with primary care teams, consultants and allied health professionals during a series of projects and placements - in general practice, outreach clinics, community hospitals and care facilities.
You will of course spend time in hospitals – for example on medical and surgical wards, from specialised cancer treatment centres and psychiatric in-patient units, to labour wards and research laboratories - but from your first weeks as a medical student you will meet patients in general practice and start to join them on their healthcare journey.
While on campus you’ll study in small groups with our team of experienced medical doctors, using a ‘problem based learning’ approach that builds complexity year-on-year.
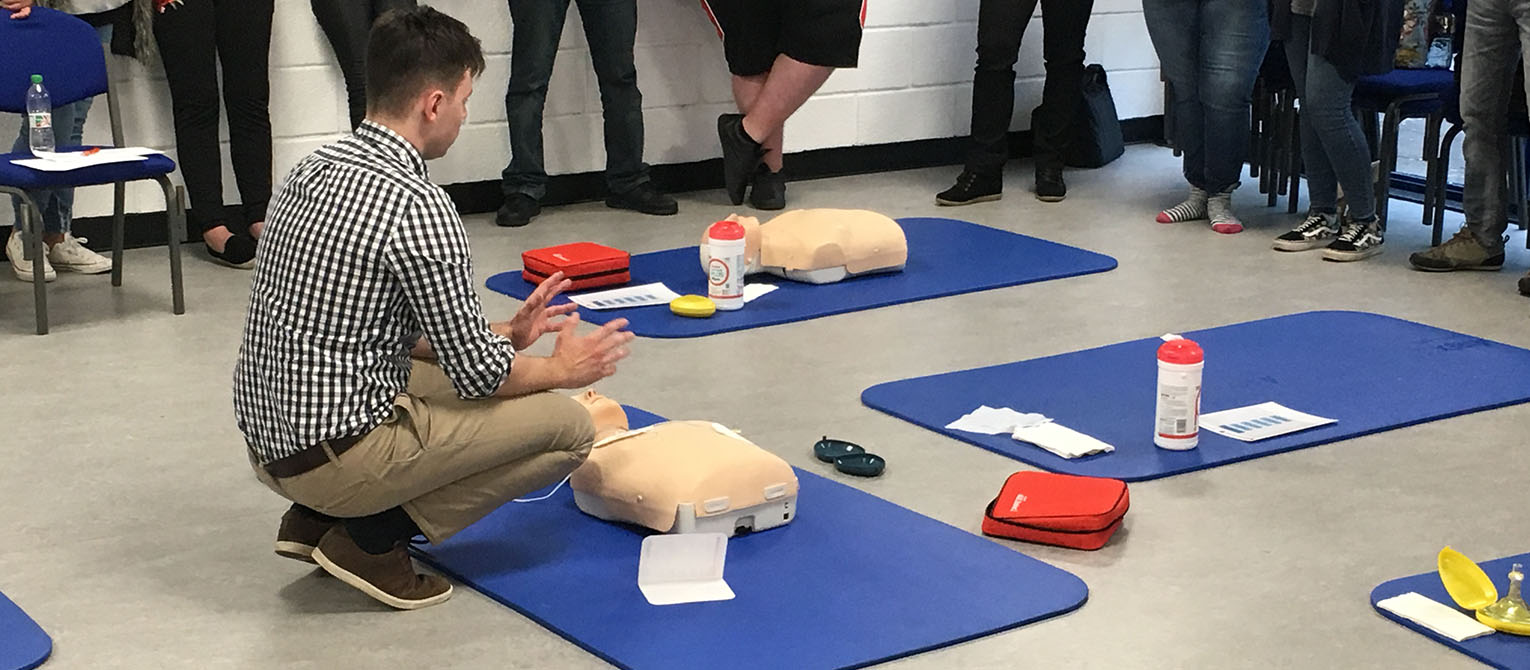
You’ll be based on our new health and wellbeing campus, working alongside students studying other health professions. The new facility includes a specialised anatomy skills room using high fidelity models for visualisation of anatomy, pathology and physiology; a simulated GP’s surgery with a suite of consultation rooms; technology for viewing and feedback space; and easily dividable units for Objective Structured Clinical Examinations.
Course content
Our MBChB course is taught over four years and divided into two phases.
We regularly review our courses to reflect the latest research and developments in the subject area, as well as feedback from students, employers and the wider sector. As a result, modules may change to ensure the course remains current and relevant.
Careers
After graduating from the Three Counties Medical School and completing the two year Foundation Programme, you’ll be in a position to apply for posts within your chosen speciality. For most these will be hospital and primary care posts in the NHS, but there are also research and commercial opportunities in fields such as the pharmaceutical industry, law and the media.
What is the Foundation Programme?
The UK Foundation Programme is a two-year, work-based training programme which is intended to bridge the gap between medical school and specialty or general practice training.
As a graduate of our MBChB you will be in a position to provisionally register with the GMC (providing you meet all of the GMC's Fitness to Practise guidelines) and apply to become a Foundation Year 1 doctor. Access to the Foundation Programme is competitive and subject to you meeting all the eligibility criteria. After that you will be working primarily in hospitals to consolidate your knowledge.
Foundation Programmes are run through Foundation Schools. In the Three Counties area these are the West Midlands South Foundation School, covering Herefordshire and Worcestershire, and the Severn Deanery Foundation School, covering Gloucestershire.
International students
As an international applicant it is your responsibility to ensure that the University of Worcester MBChB, which will be your Primary Medical Qualification (PMQ) upon graduation, satisfies the requirements of the country in which you wish to work.
Course highlights
Teaching and assessment
Our MBChB programme is developed according to the General Medical Council Outcomes for Graduates (2018). These outcomes describe what a graduate from this course is expected to be able to demonstrate.
Teaching and assessment contents
As a graduate, you’ll know the importance of self-directed learning. You’ll be taught by patients, doctors, and other members of the healthcare team (in addition to basic and applied scientists), and it will be up to you to make the most of these valuable learning opportunities.
All your teaching and learning activities, including assessments and work-place-based assessments, will be documented in an e-portfolio, where you will be required to reflect on your progress towards the Outcomes for Graduates.
The learning opportunities that enable the development of these outcomes might occur at planned and unplanned times and in expected and unexpected ways. The best teachers are the patients, but they do not arrive in accordance with the curriculum, so you will be expected to be flexible and seek out the maximum experience from the learning opportunities.
This means that although many opportunities are designed, others, and perhaps the most valuable, will be opportunistic and they just happen. The curriculum is ‘spiral’ which means that certain topics or areas might come up time and again and as you travel around the spiral, you will broaden and deepen your understanding. The responsibility for this developmental progress is ultimately yours as the student, although we will certainly do everything we can to ensure you have all the facilities, support and opportunities you need to achieve your goals.
Studying at Worcester
Entry requirements
The MBChB course at Worcester is a graduate-entry programme. To be considered you will:
- hold, or be expected to achieve in the year of application, a 1st or 2:1 undergraduate honours degree in any subject (or 2:2 plus Masters or Doctoral degree)
- have passed GCSEs (or equivalent) at grade C/4 or above in Maths and English
- not have previously commenced a medical degree in the UK or overseas
If your degree is in a non-Science subject you will also need to:
- have passed GCSEs (or equivalent) at grade C/4 or above in two science subjects (maths is not included as a science subject)
Any questions?
If you have any questions about entry requirements, please call our Admissions Office on 01905 855111 or email admissions@worc.ac.uk.
Fees
Fees contents
Home students
You will be charged tuition fees for each year of study, which will be £9,790 in 2026/27. Tuition fees generally increase each year with inflation.
Financial support is available for eligible students, however the amounts have not yet been confirmed for 2026/27. For 2025/26 the support was as follows:
2025/26 Funding for Year 1
You are responsible for paying the first £3,571 of the tuition fee yourself. Eligible students can then apply for a tuition fee loan of up to £5,964 to cover the balance of the fee, from Student Finance (this loan is not means tested).
You may be eligible to take out a loan towards living costs of up to £10,544. £4,915 (of the loan is non means tested; the remainder is means tested on household income. The loan is lower if you live with your parents during term time.
You can apply online for both the tuition fee loan and maintenance loan via the Government’s student finance website.
Depending on your circumstances you may be eligible for supplementary grants from Government Student Finance, such as: Adult Dependants Grant; Childcare Grant; and Parents Learning Allowance.
2025/26 Funding for Years 2 – 4
Tuition fees are partially paid by the NHS. You can apply to Student Finance for a tuition fee loan to pay the balance of the tuition fee.
The NHS provides a non means tested grant of £1,052 and a means tested bursary towards living costs (you are advised to check current year rates as these may change year to year). The means tested bursary is lower if you live with your parents during term time. Please visit the NHS Bursary website for full details.
Eligible students can also apply for a reduced rate, non means tested, loan of £2,753 (non final-year rate) from Student Finance. This is lower if you live with your parents during term time. The loan is also lower for the final year of the course.
The NHS pays additional allowances depending on your personal circumstances (similar to those offered by Government Student Finance in year 1): Childcare Allowance; Dependants Allowance; and Parents Learning Allowance.
The NHS also provides the Disabled Student's Allowance for these years.
International and EU students
The fees for International and EU students enrolling in the 2026/27 academic year are £49,300 per year.
Tuition fees are reviewed annually and may increase during the course. For more details, please visit our course fees page.
How to apply
How to apply contents
Applying through UCAS
Bachelor of Medicine and Bachelor of Surgery MBChB - A101
UCAS is the central organisation through which applications are processed for entry onto full-time undergraduate courses in Higher Education in the UK.
Read our How to apply pages for more information on applying and to find out what happens to your application.
Please note: If you have already taken the UCAT or GAMSAT test, it is important that you include your test result in the 'Qualifications' section of your UCAS form. This will help avoid delays in processing your application and shortlisting for interview.
We are still open to applications from international students for September 2026 entry.
Contact
If you have any questions, please get in touch. We're here to help you every step of the way.
Admissions Office
admissions@worc.ac.uk01905 855111More to explore
Open Days
Visiting us is the best way to get a feel for student life at the University of Worcester.

The City of Worcester
Worcester is a welcoming university city with great transport links and plenty of student parking.

Accommodation
Benefit from our accommodation guarantee. We have rooms on campus to suit every budget including en-suite options.